In 2020, my then 17-year-old intensely autistic, non-speaking son, Caoimh (“keev”), lost consciousness and fell down convulsing. I wasn’t with him at the time, but what he experienced was intensely disturbing.
It set him on a challenging journey of trying to navigate the health system as an autistic person.
During his toddler years, I’d seen Caoimh have staring spells. And by the age of 14, his injurious outbursts had become so dangerous to himself and his family that he required residential care.
Now I worried that both the staring spells and the outbursts were epileptiform in nature, and that Caoimh may have been experiencing unrecognised seizures for years.
The first step was to get Caoimh checked for anything brain-structural that might be causing his seizures, and for possible seizure-related brain injury. Most neurotypical people diagnosed with epilepsy routinely have an MRI brain scan to rule these out. Many autistic people, on the other hand, do not have an MRI as part of their epilepsy investigation – because they have neither the advocacy nor the extra support required to get the procedure achieved.
Lots of us would find it a challenge to lie still in a claustrophobic, racket-making tube for 20 minutes while our brains were imaged. For an autistic person who has both emotional and sensory stress, and who is also, like Caoimh, apraxic – ie, unable to control movement because of neurological brain-body disconnect – getting an MRI, and that all-important blood test, may be out of the question unless it’s under general anaesthetic.
Even giving consent, and allowing him the space to ask questions, is complex.
Fortunately for Caoimh, I’d stubbornly ignored professional opinion that his intelligence was so low that understanding even basic language was beyond him. I persisted in my hunch that Caoimh’s problem was one of output, not input; and that his apraxic brain-body disconnect was creating a “locked-in” effect, given that all communication depends on purposeful movement. Caoimh was 11 when I finally found the spell-to-communicate (S2C) approach that eventually, over an 18-month daily practice period, unlocked him into the ability to fully – if slowly, and with immense effort – express his beautifully complex thoughts, by pointing at letters on a letter board. I shudder to think what Caoimh would be enduring now – as an adult who needs to communicate with a large medical team – had I believed the prevailing dogma that “not speaking is the same as not thinking”.
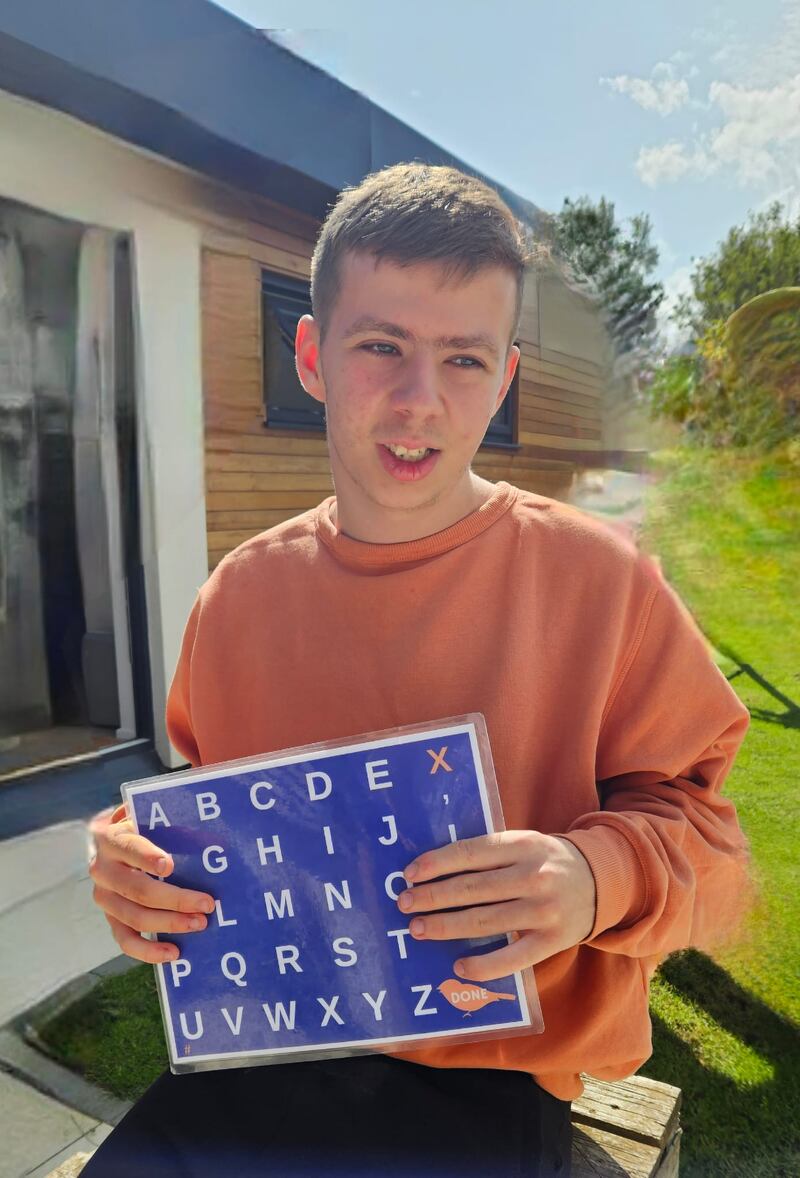
Now we’re clear on how crucial it is that non-speakers are taught the arm-movement necessary to point accurately at letterboards (a process that, like learning an instrument, takes daily practice over at least a year, until proficient muscle memory is achieved), I’ll return to our prep for that MRI and blood test under general anaesthetic.
For Caoimh to get his MRI, and the blood test that would finally give us a diagnosis he needed a wide range of additional support and planning, way beyond what neurotypical patients require. The list of what needed to be done so he could get the MRI was long, starting with a programme of education about why we were advising an MRI and a blood test under general anaesthetic, and what they involved. He needed a way to ask questions about, demonstrate his understanding of, and communicate his consent for the procedure, given that he can’t speak. Weeks of preparation and reassurance by his residential support staff, his dad Dara, and me. Photos and videos of the hospital, outside and in. Photos of people in hospital gowns and masks. Lots of discussion, planning and co-operation between us as advocates, and Caoimh’s neurologist and the hospital ward. The presence of two support staff with him on the day. As little as possible waiting time once in the hospital, and a quiet, secluded place to wait. An oral sedative. For me to be the one to hold a gas mask over his nose and mouth (having dummy-run this multiple times).
On the day, thanks to all the preparation we had done together, he managed – heroically – to control his movements.
Without this level of team effort and planning, it would not have been possible to rule out a brain injury or tumour in Caoimh. Nor would we have discovered, by requesting genetic screening of his bloods, that Caoimh has Bardet Biedl Syndrome (BBS) – a rare and complex degenerative genetic disease that requires him to be closely medically monitored for the rest of his life. Now we understand that Caoimh’s disabilities, and his physical and mental health difficulties, stem from BBS.
If we’d never found out about the BBS, Caoimh risked falling into vision loss, diabetes, obesity, kidney disease and a host of other potential dangers, with us having no idea why any of it was happening, and no heads-up in trying to manage it.
Now aged 20, Caoimh has appointments in neurology, respiratory, psychiatry, endocrinology, ophthalmology, nephrology, and gastroenterology, and we find ourselves at the coal face of how autistic patients experience the Irish medical system.
I ask the many medical secretaries that I talk to for photos of their hospital places and people; to ensure zero wait time; and an email listing the clinical questions that the consultant would normally ask a speaking, neurotypical patient (weeks in advance, to give Caoimh the time he needs to spell-to-communicate about his symptoms).
Sometimes I’m met with a willingness to help make the appointment a success. Other times my requests provoke resistance, like I’m a pushy, pain-in-the-ass mother of an annoyingly awkward patient.
We recently had a fantastic consultation with a Dublin epilepsy team. A manager took us under her wing weeks before the appointment, going out of her way to do the extra preparation required to set us up for success. She ensured that we had the first appointment after lunch so there was no waiting, and met us in the busy hospital lobby to shepherd us through.
This compassionate and practical manager primed the epilepsy specialists about Caoimh’s S2C method, and his need for the presence of his S2C communication and regulation partner Anna Lechleiter, in the room. They were ready to give Caoimh the extra time he required to describe his pre-seizure symptoms. Caoimh’s words enabled the specialists to pinpoint the type of epilepsy he has, without having to resort to a sensorily-stressful and likely impossible EEG.
But such accommodation for autistic patients is far from given. It depends on the patient having a strong team of advocates and supporters; the ability of those advocates to educate and cajole; and individual kindness.
From the Government’s June 2023 Final Report of the Joint Committee on Autism, it’s clear that the barriers to equality in healthcare faced by autistic people amount to a serious breach of human rights, which Government should legislate to prevent.
Two straightforward, cost-effective strategies would make a massive difference: scheduling hospital outpatient clinics for autistic patients on Sundays, when overcrowded waiting rooms aren’t a problem; and (as has happened in the UK) introducing mandatory autism training for all health service staff.
These simple first steps would help make the lives of autistic patients like Caoimh, and their families, that much easier.
Do you have a First Person experience about your own life you’d like to write about? Email opinion@irishtimes.com














