Hundreds of Irish women with breast cancer are being provided with free access to a gene test that can show whether or not they will need to be treated with invasive chemotherapy.
The Oncotype test has already been made available to almost 700 women with early-stage breast cancer in Ireland, and has shown that 70 per cent in this group do not need chemotherapy.
The success of this trial has led to the test also being made available to women whose breast cancer has spread to the lymph nodes. It is expected about 300 of the 650 patients a year with this condition will qualify for access to the Pondx programme, which closed at the end of May.
While the prognosis for women with node-positive breast cancer is worse than for women whose cancer has not spread, it is expected the test will show up to 40 per cent of these women will not need chemotherapy.
The development comes as the latest research results for the Oncotype test confirm that most women with early-stage breast cancer do not benefit from chemotherapy and can be treated with hormone therapy alone.
For 70 per cent of women with HR-positive, HER2-negative, node-negative breast cancer, chemotherapy confers no benefit, findings from the Trial Assigning Individualised Options for Treatment (Tailorx) international study indicate.
Lymph nodes
"We're getting new data all the time from the research, confirming the cost-effectiveness of the test," said Dr Janice Walshe, a consultant medical oncologist at St Vincent's University Hospital in Dublin, speaking from the American Society of Clinical Oncology (Asco) annual scientific meeting in Chicago,.
“Tailorx has shown the benefits among women with node-negative disease, but I believe we’re going to see similar benefits now for women who have breast cancer in the lymph nodes,” said Dr Walshe.
Chemotherapy works best where cancer cells are dividing quickly, she pointed out, so in those tumours that are growing more slowly, hormone therapy is often more effective and chemotherapy “adds nothing”.
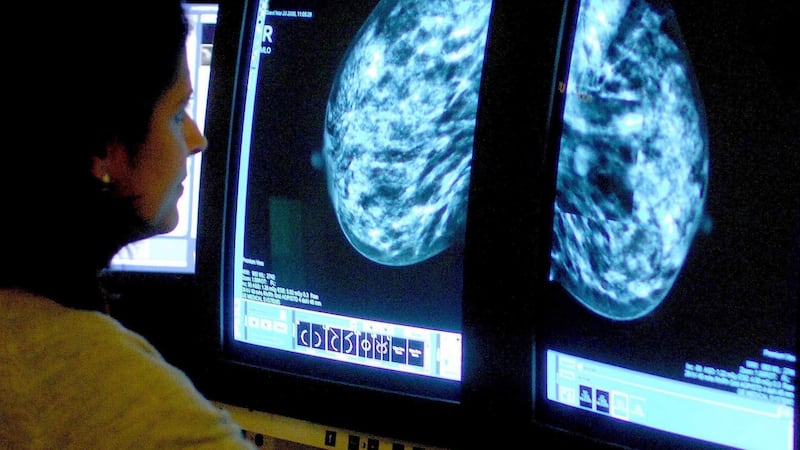
Tailorx, which uses the Oncotype gene test to optimise treatment for women with breast cancer after surgery, has enrolled more than 10,000 women in six countries, including 700 in Ireland. With the test, a tumour sample is tested after surgery for 21 genetic markers, which indicate if it could grow and spread.
The test assigns a risk score between 0 and 100 based on cancer recurrence. Based on evidence from earlier trials, women who had a score in the low-risk range (0-10) received hormone therapy only, and who with a score in the high-risk end (26 and above) were given therapy to block the oestrogen hormone, and chemotherapy.
Disease-free survival
Women in the trial who had a score in the intermediate range (11-25) were randomly assigned to receive hormone therapy alone or hormone therapy with chemotherapy. The goal was to assess whether women who received hormone therapy alone had outcomes that were as good as those among women who received chemotherapy in addition to hormone therapy.
The researchers found that the primary endpoint of the trial, invasive disease-free survival, was very similar in both groups.
Five years after treatment, the rate of invasive disease-free survival was 92.8 per cent for those who had hormone therapy alone and 93.1 per cent for those who also had chemotherapy. The difference is not statistically significant.
The researchers also found that women with a score of 0-10 had very low recurrence rates with hormone therapy alone at nine years (3 per cent). This confirms similar findings from earlier studies.
In addition, they found that women with a score of 26-100 had a distant recurrence rate of 13 per cent despite receiving both chemotherapy and hormone therapy. This finding indicates the need to develop more effective therapies for women at high risk of recurrence.
Researchers identified one caveat to their findings. For pre-menopausal women and those younger than 50 years old at the higher end of the intermediate-risk range separately, the results showed there may be a small benefit from chemotherapy.
Oncotype genetic test: How one woman discovered she did not need chemotherapy
Gene testing for cancer patients was in its infancy when Linda Hannan received her diagnosis of the disease back in 2010.
“They discovered something wrong with the breast, and performed a lumpectomy. Of course, you’re devastated, you don’t know what lies ahead,” says the mother of two from Celbridge.
Further treatment was recommended and in this oncologists tend to err on the side of caution so as to minimise the risk of recurrence.
Hannan’s doctor recommended six months of chemotherapy, with radiotherapy to follow, but just at this time she heard about the Oncotype genetic test then in development.
From an examination of tumour tissue, it builds up a picture of the likelihood of recurrence, based on the expression of 21 genes associated with breast cancer in the sample. Patients are given a score ranging from 0 to 100 based on the risk of recurrence, and for some with low scores hormone therapy may suffice.
With the test not freely available in Ireland at the time, Hannan had to pay €3,000 privately to have her tissue sample examined in the US.
The results that came back placed her in the low-risk (0-10) category for recurrence. This meant she didn’t need chemotherapy, and was able to move straight to a bout of radiotherapy.













