What is it and who gets it?
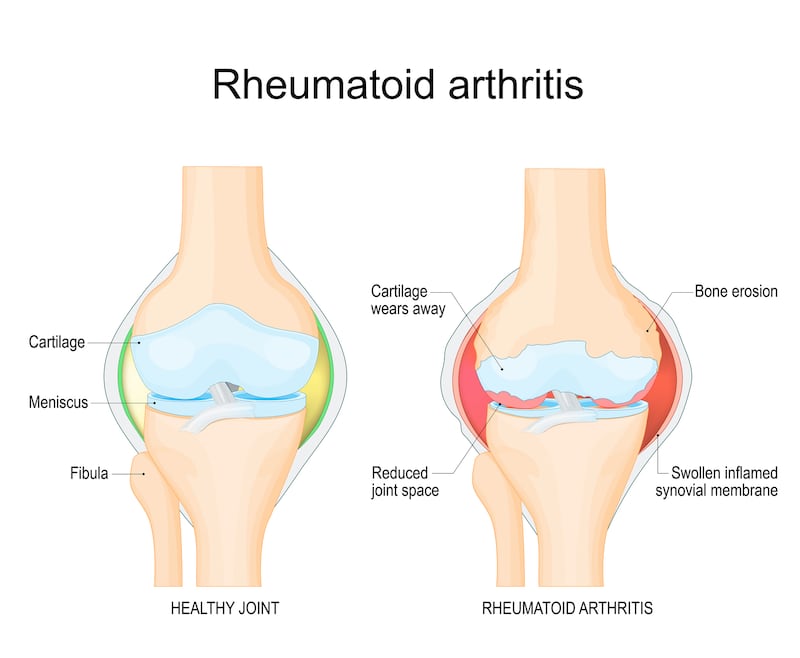
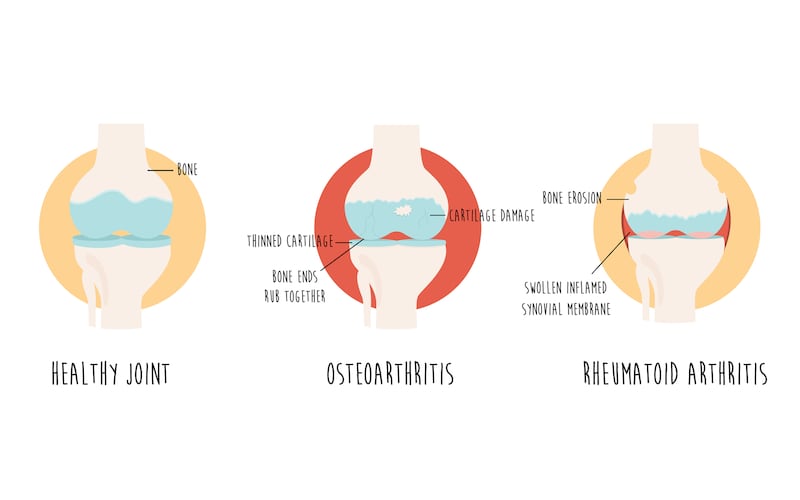
Rheumatoid arthritis is an autoimmune condition which causes inflammation to the joints resulting in pain and stiffness. If left untreated, the inflammation will damage the cartilage and bone in the affected areas of the hands, wrists, knees, hips, feet and ankles, shoulders or lower back.
Rheumatoid arthritis can develop at any stage in life (eg, juvenile arthritis is a form of rheumatoid arthritis) with one in 100 people suffering from it in this country. It is more common in women than men. Although the precise cause of rheumatoid arthritis is unknown, a small number of genes predispose a person to rheumatoid arthritis. Smoking also increases the risk of getting it.
Not to be confused with the more common osteoarthritis – which is a degenerative joint disease due to “wear and tear” of the joints – rheumatoid arthritis develops because the body’s natural self-defences (the immune system) attack healthy tissues.
“With rheumatoid arthritis, people feel stiffness in the small joints of the hands and feet in the morning time, whereas osteoarthritis occurs in older people, a younger person who had a trauma to their joint or due to a congenital abnormality,” explains Prof Gaye Cunnane, consultant rheumatologist at St James’s Hospital, Dublin and clinical professor of rheumatology at Trinity College Dublin.
RM Block
What are the symptoms and how is it diagnosed?
The symptoms of rheumatoid arthritis are swollen joints which are stiff and painful. Feelings of fatigue similar to having influenza are also a common symptom. “Some people come down with rheumatoid arthritis overnight while others experience worsening symptoms over time. For some people, the aches and stiffness disappear and come back again in a condition we call palindromic rheumatism. Over time, the symptoms will become consistent,” says Cunnane.

Diagnosis of rheumatoid arthritis requires a rheumatologist to take a very detailed history of symptoms coupled with a physical examination of the joints and other areas of the body. Blood tests are carried out to check for the presence of biomarkers of inflammation or to rule out other conditions. X-rays of the hands and feet or ultrasound or MRI can provide evidence to back up clinical diagnosis if necessary.
What treatments are available and are they different from earlier treatments?
Methotrexate is the standard medication for rheumatoid arthritis and rheumatologists say that when it works, it can put patients into a remission of their symptoms within a few months of taking the drugs. The introduction of biologic therapies which target the T-cells, B-cells and specific cytokines (proteins) in the immune system have heralded a new era in the treatment of rheumatoid arthritis.
“What we tend to do is put patients on methotrexate initially and if there is a response from it, this is the best-case scenario. If there hasn’t been a good enough response, we will add a biologic as our aim is complete remission of symptoms,” says Cunnane. “Early diagnosis is key so the joints can be treated before they become deformed. We rarely see cases of deformed joints now with these new treatments,” she adds.
In the mid-20th century, the discovery of steroids was deemed a miracle treatment for rheumatoid arthritis. However, over time, experts realised they were not a long-term treatment as, while they improved the symptoms, they didn’t treat the underlying mechanisms which caused the inflammation. Steroids are still used for short periods of time (four-six weeks) while waiting for the disease-modifying medication to start working.
“Sometimes people think they can stop taking the disease-modifying drugs when they don’t have any symptoms, but we explain that rheumatoid arthritis is a lifelong disease and the medication is needed even when people are feeling well,” says Cunnane.
It’s important for people with rheumatoid arthritis to have a healthy diet, keep their weight under control, limit their alcohol consumption, not smoke and take sufficient exercise. “Rheumatoid arthritis is not a curable disease, but we can put it in remission so that people can live normal lives,” she says.
Have there been any breakthroughs in the understanding and management of the condition recently?
The arrival of the aforementioned biologic disease-modifying drugs in the early 2000s, followed by biosimilar drugs some years later, have been game-changers in the treatment of rheumatoid arthritis.
While biologics (drugs made from substances which occur in nature – produced by a biological rather than chemical process) are very expensive drugs, the arrival of their cheaper cousins, biosimilar drugs, has reduced their price somewhat. Treating patients with these immunotherapy drugs has also meant that the majority of people with rheumatoid arthritis remain healthy, reducing hospital stays hugely. Less than 1 per cent of patients coming through emergency departments have rheumatology diseases now.
“There are very few rheumatology patients in hospital now”, says Prof David Kane, consultant rheumatologist at Tallaght University Hospital and HSE national clinical lead for rheumatology.

“Before we had biologics, 50 per cent of people with rheumatoid arthritis would be out of work within five years, now over 90 per cent of people remain in work.”
What are the health services like for people with rheumatoid arthritis?
Kane says the ideal is for rheumatologists to see all patients with rheumatoid arthritis referred by GPs at an outpatients clinic within six weeks, although this isn’t the case in all hospitals. “We currently have 60 consultant rheumatologists with the aim to have 80 by 2028. We try to fast-track patients with the highest illness burden. We have a form for GPs which identifies all the key symptoms which, if embedded into the referral, would make it easier to identify patients with the greatest need for these rapid access clinics,” he adds.
Arthritis Ireland runs free self-management programmes for people with all forms of arthritis. These programmes help people manage their medications, keep physically active, deal with the psychological aspects of the disease and communicate well with health professionals. The Arthritis Ireland free confidential helpline is 0818 252 846 and the email is helpline@arthritisireland.ie. A booklet on living with rheumatoid arthritis can also be downloaded from its website.
What does the future hold for people with rheumatoid arthritis?
Rheumatologists expect that medications will become more precise and personalised as increased knowledge about the presence of antibodies such as rheumatoid factor and anti-CCP and specific cytokines in blood are already helping clinicians choose more targeted medications for individual patients.
A significant percentage of people with RA don’t respond well to treatment. But researchers at TCD, along with St Vincent’s University Hospital, are identifying biomarkers in inflamed tissue of people with rheumatoid arthritis which, they hope, will predict which treatment suits which patient at diagnosis.
“We hope to develop blood tests which will allow clinicians routinely identify the right treatment for the right person from onset of disease. Our research is also looking at ways to identify new therapies for patients who don’t respond to any treatment, in addition to studying individuals at risk of developing rheumatoid arthritis to enable earlier diagnosis and treatment,” explains Ursula Fearon, professor of molecular rheumatology at TCD.
There is also an expectation that implantable devices will be able to detect cytokines and predict and treat a relapse of symptoms before it sets in.
“Wearable devices which monitor blood, sweat, urine and even voice patterns [eg hoarseness] will give early indication of disease onset or relapse. And, artificial intelligence will be able to analyse this data with data from the genome and radiology to provide even more information,” says Cunnane.
















