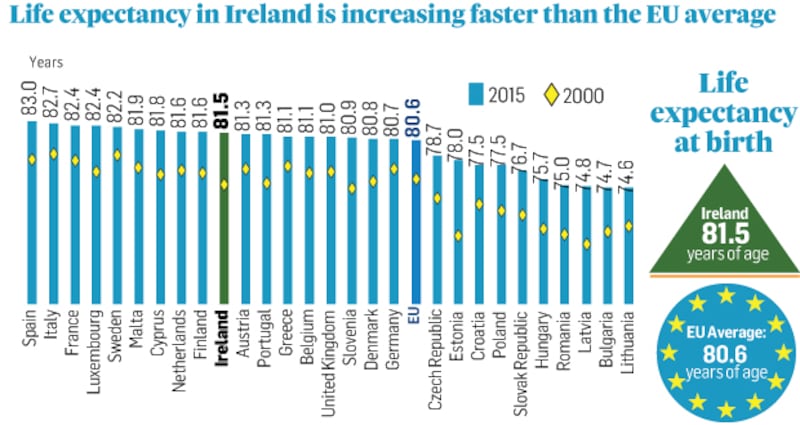
Men and women in Ireland are living on average a remarkable five years more today than they were in 2000 (now, to 81.5 years).
That’s just above the EU average (80.9), although Irish women still continue to have the edge on men by four years.
And there is still also a gap of eight years in the life expectancy between EU citizens of western Europe and those of central and eastern Europe – the European Union is yet far from "one".
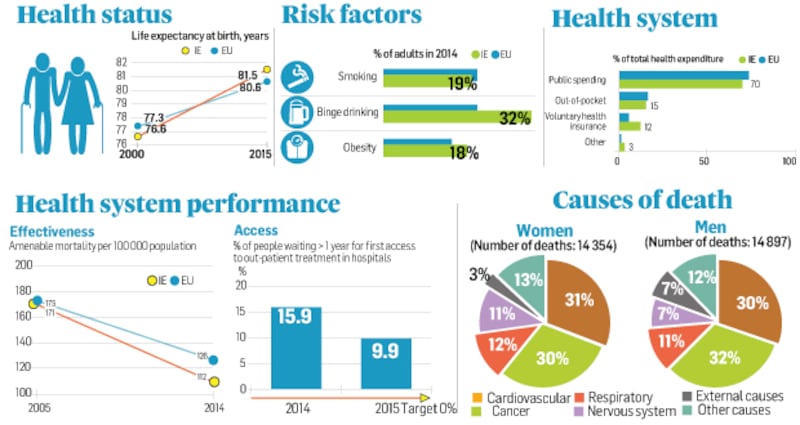
The gains in life expectancy in Ireland have been largely driven by a reduction in the mortality rate for cardiovascular diseases, which were nearly halved between 2000 and 2014.
In no small measure these reflect the successful work of our much-maligned health system, the subject of a major new comparative OECD/EU study, State of Health in the EU, which looks at healthcare in the individual member-states of the union (data only up to 2015-16). The study was compiled by the Organisation for Economic Co-operation and Development (OECD) in conjunction with the EU.
Although the EU does not have a competence in health policy, the reports are about “mutual learning and exchange of good practice”.
Overall, the report argues that Ireland’s lower than average “amenable mortality rate” – premature deaths that could potentially be avoided, given effective and timely healthcare – suggests the healthcare system “is relatively effective in treating people with threatening conditions”.
But all is far from rosy.
Although we are among the states to spend most per capita on health – more than 40 per cent over the EU average, and behind only Luxembourg, Germany and the Netherlands – Ireland remains fifth from the bottom of the EU league for the number of doctors per head (2.9 per thousand compared to 3.6 EU average).
And although we have more nurses than most member states, the number of hospital beds per capita in Ireland is half the EU average at 2.6 per 1 ,000 population in 2015 (compared with an EU average of 5.1).
The report points critically to the “two tier” model of access to Irish healthcare for sharp differences in care outcomes and life expectancy for the economically disadvanted. “Ireland is the only Western European country that does not offer universal coverage of primary care,” the report says with less than half the population (47 per cent) enjoying access to free primary care.
The eligibility criteria contribute to the high regional variation in its distribution, it says, ranging from 15 per cent of the population in an urban district of Dublin to 54 per cent in a rural region in the North of the country.
Hospital waiting times for outpatient services are particularly high by European standards – 10 per cent of patients had to wait more than a year to get first access to services in 2015.
The report pins the blame on “the relatively low bed capacity in Ireland. The low availability of beds, combined with the relatively high hospitalisation rates for conditions that should normally be treated in primary care settings, contribute to a very high occupancy rate: 95 per cent of all hospital beds in acute care are occupied on average throughout the year. This is much higher than on EU average (77 per cent) and leaves little capacity to handle emergency situations, except by postponing elective procedures.”
To meet future growing health care needs in Ireland, “one long-term challenge will be to increase the capacity of the system in terms of both human and physical resources”, the report argues.
But it acknowledges the problems associated with the “sharp reduction” in public health spending growth since the financial crash in 2008/2009 and to “serious retention problems”.
Around one in two newly trained doctors do not plan to practise medicine in Ireland, the report notes: “Poor working conditions, such as understaffing of the workplace, or expectations to carry out too many non-core tasks as well as limited career prospects in Ireland were the top reasons for those planning to emigrate or pursue an alternative career.”
The report emphasises the importance of health promotion and disease prevention to reducing mortality rates. Notable progress has been achieved in reducing tobacco consumption in most EU countries through a mix of public awareness campaigns, regulations and taxation.
Yet, more than one in five adults in EU countries continues to smoke every day.
But in 2015, 19 per cent of adults in Ireland smoked tobacco every day, down from 24 per cent in 2008.
More than one in five adults in EU countries reported in 2014 heavy alcohol drinking at least once a month. In Ireland excessive alcohol consumption was well above the EU average, with 32 per cent of adults reporting having had at least six drinks in a single occasion each month in 2014.
Ireland led the EU countries in 2000 with an average annual consumption of 14.2 litres of alcohol per adult, drinking over three litres more than on average across the EU. This consumption level has gone down to 10.9 litres per capita in 2015, now only one litre above the EU.
But one in six adults across the EU, one in four in Ireland, was obese in 2014, up from one in nine in the EU in 2000.
Ageing, combined with tight budgetary constraints, will require profound adaptations to the health systems of EU countries to promote more healthy ageing and “respond in a more integrated and patient-centred way to growing and changing health care needs”.
On average across EU countries, the share of the population aged over 65 has increased from less than 10 per cent in 1960 to nearly 20 per cent in 2015 and is projected to increase further to nearly 30 per cent by 2060.
From 65, Irish men and women can expect to live only about 60 per cent of their remaining years of life free of disability, the report warns. And, as in many other EU countries, the number of people dying from Alzheimer’s and other dementias has gone up drastically. It is now one of the leading causes of death.
In making the case for increased health spending, the report points out that some 3.4 million die throughout the EU every year from non-communicable diseases, a potential loss every year of €115 billion a year in economic terms.
More than 1.2 million people in the EU died in 2013 from illnesses and injuries that might have been avoided through more effective public health and prevention policies or more timely and effective health care.
An academic study of the return on investment in health suggest a return on health investment of €14 for every €1 invested.















